This is the first of several articles about COVID-19 and related topics by Dr. Jon Crosbie, an ISU alum, sports fanatic and all-around awesome Doctor of Osteopathic Medicine.
I’d like to write something deadly serious. I know, I know, I’m usually one who spouts nothing but good vibes. But this is important. Please share.
Here’s the problem with COVID-19 and why this is different from SARS or influenza or other things we’ve dealt with. The phrase “perfect storm” is a tired and overused metaphor, but it’s unfortunately incredibly apt because of the way the virus behaves and the response by some countries, including the United States.
From a disease spreading standpoint, COVID-19 differs from SARS and influenza in two very important ways.
Difference #1. Incubation time. Incubation time is the time that the virus is spreading in your body but you don’t have any symptoms yet. And during this incubation time, you can be “shedding virus.” This is a fancy way of saying you’re contagious.
The incubation time of influenza is around 1 day. This means that people find out they’re infected very quickly and stay home. The incubation time of COVID-19 is anywhere between 2 and 14 days. This means that somebody could be walking around for up to 2 weeks, with no symptoms, shedding virus and being contagious (that’s sort of redundant but whatever).
COVID-19 also differs from influenza in the sense that it’s quite a bit more deadly. If you catch COVID-19 you are decidedly more likely to die, even if you are younger. The stats on this are still a work in progress.
Difference #2. Variable presentation. See, SARS patients were all really, really sick. Even if you didn’t have tests available, you had a high “index of suspicion” when you saw a patient with SARS. This means that you would see a SARS patient and say “oh $@%, that guy’s really sick. We haven’t tested him yet, but we better isolate him just in case.” Then you test him and find out he has SARS, but since you had him isolated just in case to begin with, it was okay.
COVID-19 patients are not all sick. Some of them, obviously, are sick as hell. But many of them are not. Many of them think (not unreasonably) they simply have a cold. And so they go about their daily lives, using pin pads at the grocery store, holding gas station pumps, serving drinks and foods…even treating patients.
Difference #2.1 (maybe) It would appear that COVID-19 is heartier than other viruses like it. COVID-19 is enveloped. Getting into the specifics of this would lengthen out this post a little too much, but most enveloped viruses don’t last beyond 24 hours out in the environment. It would appear COVID-19 lasts longer than that on certain surfaces. Now, these surface trials are all under ideal-for-virus-viability conditions, but it is very reasonable to assume that COVID-19 is heartier and lasts longer in the environment than other viruses like it.
Now, there’s one other thing that makes COVID-19 the same as SARS and different than influenza. Right now, for COVID-19 (and SARS) we have one treatment — oxygen. That’s it. Yes, you’re hearing about different drug trials, Z-Paks and hydrochloroquine…these are NOT miracle drugs. They may improve outcomes in some patients, but understand this:
If you get really sick with COVID-19, you need oxygen. You may even need a ventilator which is a machine that breathes for you if your lungs get overwhelmed.
And herein lies yet another problem — some places don’t have enough ventilators. If you’re sick as hell with COVID-19, and there’s no ventilator available to you, hydroxychloroquine and a Z-Pak is not going to save you. Quite honestly, the ventilator may not save you, either.
You must understand one other thing. We were effectively screwed on Valentine’s Day.
With a virus that behaves like COVID-19 does — the variable presentation, the incubation time and shedding of virus without symptoms — the most important information we needed was who had it and who didn’t back in February. We needed to know THEN who was walking around with mild cold symptoms and who was shedding virus out in the community so we could stop the spread and take the most important step that existed to flatten the curve you’ve heard about.
We did not know this. And, because of the way the virus behaves, and because we didn’t test people aggressively, widespread community transmission started to occur.
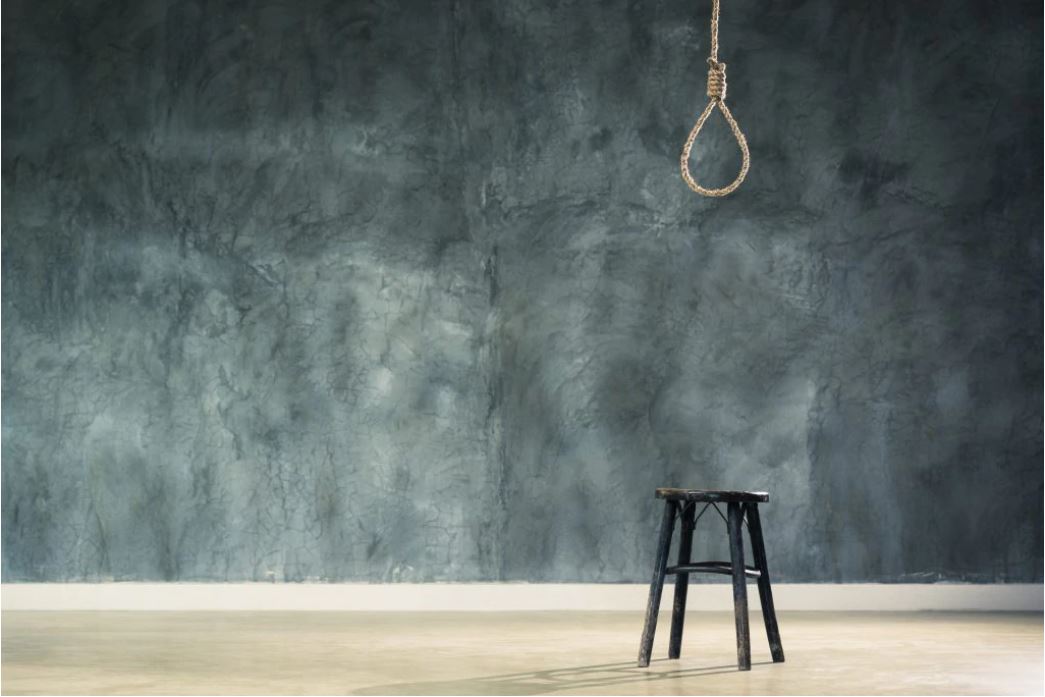
Not testing everybody in February was akin to sauntering up to a gallows, stepping up onto the stool, and slipping our collective neck into a noose. With current projections of infection, the country may be short on ventilators as well as having a generally overwhelmed medical system in some places very shortly. It happened in New York. They had to bring in an extra boat-hospital, for God’s sake. If you’re living in middle America or down in Georgia or some other place that’s decided to relax social distancing, think very, very hard about going out.
The gallows metaphor is very appropriate. Just having your neck in the noose will not kill you. You still have to step off the stool.
If we can just stay put, we don’t step off the stool. Going to the movies, to the mall, to sporting events, to school was stepping off the stool. Each time you go to the grocery store, you have one foot off the stool. Each time you make an unnecessary trip out, you risk falling off the stool. IF YOU MEET WITH FRIENDS AND RELATIVES THAT DON’T TAKE THIS SERIOUSLY, YOU HAVE ONE FOOT OFF AND THE STOOL IS WOBBLING LIKE CRAZY.
At this point, it’s up to you to stay on the stool. Now, you may get COVID-19 and be like Tom Hanks or Kevin Durant and be just fine. But you may not. You may develop a high fever and pneumonia. Your oxygen saturation may drop and you will be unable to breathe because your lungs are flooded. The only thing that can save you then is a machine that breathes for you while your lungs try to fix themselves, if there’s one of those machines available. And that machine might not be able to do shit for you, anyway.
Don’t get it twisted — there is a noose around all of our necks right now.
Dr. Jon Crosbie, D.O., is a Physician and Assistant Professor at Des Moines University Medical School